#298 The Atrial Fibrillation Diet: How to Beat A-Fib with Food
December 12th, 2018 by Dr. John DayThe Atrial Fibrillation Diet: How to Beat A-Fib with Food
A lifetime of poor eating choices is one of the leading causes of atrial fibrillation that I see in my cardiology practice. Wouldn’t it be great if there was an atrial fibrillation diet that could reverse atrial fibrillation without the need for drugs or procedures? In this article, I’ll share the science behind the Atrial Fibrillation Diet and teach you everything you need to know to beat atrial fibrillation with food.
7 Ways What You Eat May Cause Atrial Fibrillation
1. Excessive Pericardial Fat
There are two main places where fat is stored in the body. It can be stored under your skin or around your internal organs. When it is stored internally, it is called visceral fat. Of these two places where fat is stored, visceral fat is by far the most dangerous. And of all the places where you could have visceral fat, fat encasing the heart or pericardial fat is the worst place for your long-term health and atrial fibrillation risk.
The pericardium is a thin membranous sack holding the heart. Sometimes, the pericardial fat layer surrounding the heart can be more than an inch thick!
Fat cells, especially the visceral pericardial fat wrapping around the heart, release cytokines into the heart. Cytokines are small proteins that activate the immune system. And this immune system activation from cytokines leads to an intense inflammatory reaction which scars up the heart and may cause atrial fibrillation. Thus, the less pericardial fat you have encasing your heart, the less inflammation and scarring you will have going on inside of your heart.
So how do you know if you have too much visceral or pericardial fat? While an MRI or CT scan could definitely tell you how thick your pericardial fat layer is, doing these tests probably isn’t the most practical option for most people. Fortunately, there is an easier way. Studies show that your waist circumference is an excellent predictor of how much visceral fat you have. And to beat atrial fibrillation, research indicates that men want to get their waist size down to 35 inches. For women, your goal waist size to prevent and reverse atrial fibrillation is 32 inches.
2. Insufficient Antioxidants

Oxidation is the same chemical reaction that causes iron to rust. In the body, oxidation is one way in which the body ages.
Aging of the heart is one of the most powerful causes of atrial fibrillation. This is why it is so common to see seventy or eighty-year-olds with atrial fibrillation. Indeed, based on our research at Intermountain Medical Center, atrial fibrillation can be thought of as premature aging of the heart. And to stop this oxidation aging process, you need more antioxidants from food.
Another mechanism whereby insufficient antioxidants may lead to atrial fibrillation is through excessive production of reactive oxidant species. Indeed, these reactive oxidant species like myeloperoxidase, nicotinamide adenine dinucleotide phosphate oxidase, and uncoupled nitric oxide synthase enzymes have been shown to disrupt electrical pathways in the heart. With enough antioxidants in the diet, overproduction of reactive oxidant species can be stopped.
Antioxidants are food compounds which block this oxidation aging process and reactive oxidant species. For example, one study of 800 people showed that those who got the most antioxidants from vitamins like C, E, and carotenoids from vegetables and fruit were twice as likely to have their hearts go back to normal rhythm without drugs or procedures. Just to be clear, antioxidant dietary supplements have never been shown to prevent atrial fibrillation. You can only get this antioxidant atrial fibrillation benefit by eating massive quantities of real food, especially vegetables.
3. Unnecessary Inflammation
Inflammation or activation of your immune system is definitely needed if you are injured or fighting an infection — however, low-level inflammation that is always present and never turned off damages your heart. Indeed, anything that causes chronic low-level inflammation in your body may increase your risk of atrial fibrillation. This is because unnecessary activation of your immune system causes the release of many inflammatory proteins, antibodies, etc. that damage heart cells and disrupt electrical pathways.
While cytokines from fat cells encasing the heart are one way that inflammation may damage the heart and cause atrial fibrillation, another way is through the diet. The daily food choices we all must make determine whether or not there is a low-grade inflammation going on within your heart.
For example, studies show that anything triggering a blood glucose spike, like sugar or flour, may activate the immune system in a way that could increase the risk of atrial fibrillation. Likewise, anything in the modern diet like processed foods, fried foods, fast foods, etc. may also trigger this same inflammation-induced damage to your heart.
To protect yourself from the inflammation damage caused by anything in the standard American diet, you need as many vegetables and fruit as possible, especially vegetables. Indeed, studies show that the more vegetables and fruit you can eat the less of this unnecessary activation of the immune system (inflammation) you will have. This, in turn, helps to prevent and reverse atrial fibrillation.
4. Micronutrient Deficiency
Micronutrient deficiency, especially that of potassium and magnesium, may also play a role in atrial fibrillation. Indeed, one study of 4,059 people showed that inadequate potassium increased the risk of atrial fibrillation by up to four times. Likewise, a study of 3,530 people showed that those with low magnesium levels were 52% more likely to develop atrial fibrillation.
The most likely reason why low potassium and magnesium levels increase the risk of atrial fibrillation is that they change the cell-to-cell electrical channels in the heart. With these electrolyte disturbances, there is cellular hyperpolarity with increased resting potential and shortening of the action potential. The bottom line is that these changes then render each cell more susceptible to electrical chaos or atrial fibrillation.
As most Americans favor processed and fast foods over vegetables, legumes, nuts, seeds, and fruit, it shouldn’t come as a surprise that most Americans don’t get enough potassium and magnesium in their diets. Surprisingly, when I talk with patients about getting more electrolytes in their diet, they often tell me that they will start drinking more Gatorade and other sports drinks.
This is absolutely the worst way to fight atrial fibrillation. These sports drinks are nothing more than sugar and chemicals with a small dose of electrolytes. Even though you can now buy these sports drinks without sugar, it still isn’t much more than artificial sweeteners and chemicals.
In addition to getting more potassium and magnesium in your diet from vegetables, legumes, nuts, seeds, and fruit, other micronutrients are also important. For example, there are studies linking atrial fibrillation to elevated levels of homocysteine (often due to a B vitamin or folate deficiency) as well as insufficient vitamin D.
5. High Blood Glucose
Increasingly, more and more studies are pointing to the importance of controlling blood glucose to prevent atrial fibrillation. For example, one study of 8,943 people showed that even if you have never been diagnosed with diabetes, but yet have an occasional borderline high glucose reading or hemoglobin A1C, you have a 33% increased risk of atrial fibrillation. And if you have been diagnosed with diabetes, then that atrial fibrillation risk goes up to 50%!
But it isn’t just whether or not you have been diagnosed with diabetes that determines your atrial fibrillation risk. For example, some studies suggest that the longer you have diabetes or the higher your hemoglobin A1C the greater your risk.
So, how does diabetes lead to atrial fibrillation? Animal studies show that even minor glucose rises, like what happens after a big meal or eating sugar or flour, causes fibrosis (scarring) of heart cells by an increase in thioredoxin-interacting protein.
6. Unhealthy Gut Microbiome/Excessive TMAO
Just as we now know that any spike in blood glucose is bad for your health, so too is an unhealthy gut microbiome. Scientists estimate that there are about 100 trillion bacterial cells living in your gut. And depending on which bacteria you have there may determine your atrial fibrillation risk.
For example, having the wrong gut bacteria may lead to a spike in a cardiac toxic byproduct called TMAO (Trimethylamine N-oxide) which can get into your bloodstream. And elevated levels of TMAO not only is linked to heart attacks but also significantly increases your risk of atrial fibrillation. Now, how TMAO damages the electrical system of the heart isn’t entirely clear but recent studies show that elevated levels of TMAO cause inflammation of the heart and damage the autonomic nervous system (the nerves controlling your heart rhythm).
If TMAO is bad for your heart, how do you stop your gut bacteria from making this stuff? Studies show that the best way to reduce TMAO is to starve off the gut bacteria that make TMAO. And to kill off these bad guys in your gut you need to limit meat, dairy, processed foods, and supplements/sports drinks containing choline and carnitine.
7. Unnecessary Enlargement of Your Heart
It has long been known that the more enlarged your atria are, the higher your risk of developing atrial fibrillation. While some enlargement of the atria may happen with age, food choices play a much bigger role.
For example, sugar and flour promote weight gain, and studies show that weight gain is the number one cause of an enlarged heart leading to atrial fibrillation. Also, high blood pressure from too much sugar and salt in the diet is another cause of unnecessary enlargement of your heart. Lastly, salt alone from processed foods may cause heart enlargement independent of blood pressure changes.
4 Ways How You Eat May Cause Atrial Fibrillation
While eating right is absolutely essential to maintaining normal rhythm, meal timing may be equally important. Below are 4 ways meal timing may prevent atrial fibrillation.
1. Big Meals May Trigger Atrial Fibrillation
Studies show that vagus nerve stimulation, like what happens when you eat too big of a meal, may trigger atrial fibrillation. For those who may have forgotten their anatomy, the vagus nerve is the tenth cranial nerve linking the gut to the heart and the brain. Thus, overstimulation of this nerve with a big meal may be all that is needed for an atrial fibrillation attack.
While the exact mechanism whereby eating a big meal leads to an emergency room visit for atrial fibrillation isn’t entirely clear, studies show that intense vagus nerve stimulation from an overfilled belly may spike acetylcholine and adrenalin levels which then renders vulnerable heart cells near the pulmonary veins to electrically fire. This abnormal electrical firing of cardiac cells near the pulmonary veins may then trigger an atrial fibrillation attack.
So how much should you eat? We could take a great lesson from the Japanese who have some of the lowest rates of atrial fibrillation on this planet. The Japanese, especially those living in Okinawa, practice “Hara Hachi Bu” which is a Confucian teaching to only eat until you are 80% full. If you never fill your belly beyond 80%, then you won’t have to worry about excessive vagal stimulation from an overfilled belly.
2. Eating Fast May Worsen Atrial Fibrillation
Just as overeating may excessively stimulate your vagus nerve, so too can eating very fast. Indeed, with fast eating, you get more stomach stretching and rapid blood glucose spikes both of which may cause an atrial fibrillation attack from vagus nerve stimulation.
Let’s face it, most of us probably eat too fast. Some simple things I like to do to slow down my eating is to focus on high fiber foods. Vegetables, especially when eaten raw, take more time to chew. This extra “chew time” with vegetables can be invaluable in preventing overstimulation of the vagus nerve.
Other tricks I employ are eating left handed. Not only will eating with your non-dominant hand slow your eating speed but it also strengthens the neural pathways in your brain by learning new skills. I have found that eating my food with chopsticks at home can also accomplish the same results. Lastly, you can always count how many times you chew your food or put your fork or spoon down between bites.
3. Cold Foods May Trigger an Atrial Fibrillation Attack
Just like overeating may trigger an atrial fibrillation attack via the vagus nerve, so too may eating cold foods. For example, one study showed that the sensation of “brain freeze” which happens from eating cold foods like ice cream or drinking cold beverages might be a potent trigger for atrial fibrillation attacks.
Does this mean you can’t ever eat ice cream or drink a big glass of ice water? Of course not. However, if you are eating or drinking cold things, the key is to do it slowly to minimize any unnecessary stimulation of the vagus nerve.
4. Intermittent Fasting May Prevent Atrial Fibrillation
Intermittent fasting may represent an exciting way to prevent atrial fibrillation through food timing. Indeed, intermittent fasting optimizes blood glucose fluctuations and vagus nerve excitability which may be quite helpful in controlling atrial fibrillation.
While there aren’t any published studies yet on using intermittent fasting to treat atrial fibrillation, when we have looked at the studies done at our hospital we are encouraged by the initial results. In a small group of 329 people, we observed a statistical trend toward a 20% to 40% reduction in atrial fibrillation regardless of how we analyzed the data. While certainly encouraging, further studies are needed to confirm if there is indeed a cause and effect relationship between intermittent fasting and atrial fibrillation.
Until further data are available, what should you do? Unless told otherwise by their other doctors, I encourage all of my patients to go 12 hours each night without eating. To accomplish this, I ask my patients not to eat after 7 PM. The reason for this is that studies show late eating may spike glucose levels and blood pressure until very early in the morning (these changes alone could trigger an atrial fibrillation attack). After “closing” the kitchen at 7 PM, they are then free to re-open the kitchen at 7 AM the next morning.
7 Ways to Beat A-Fib with the Atrial Fibrillation Diet
Now that we have discussed the science behind eating and the atrial fibrillation diet, what should you eat? Below are what we know from studies.
1. Lean Body Weight
Regardless of what you eat or how you eat it, staying a “healthy lean” may be the best protection you have against atrial fibrillation. Indeed, our studies have shown that the leaner you are, the lower your risk of atrial fibrillation. We have shown from our studies that even maintaining a five-pound weight loss can statistically reduce your long-term risk of atrial fibrillation. The key is that you need to work with your physician to achieve this goal in a healthy and sustainable way.
2. Tripple Your Veggies
If there is one superfood you want to focus on to beat atrial fibrillation, it is veggies. Many studies show that the more plant-based you can eat, the lower your risk of atrial fibrillation. Make sure veggies are a big part of every meal you eat.
Fruit, especially berries, can also be helpful in maintaining normal rhythm. Berries are your best bet as they pack the most micronutrients and are the least likely to spike blood glucose levels.
Vegetables and fruit are packed with antioxidants, magnesium, potassium, as well as the fact that they are also anti-inflammatory. All of these properties make vegetables and fruit a great choice for those wishing to prevent or reverse atrial fibrillation.
3. Eat More Plant-Based Fats

When it comes to fat in the diet, the more healthy fats you can get the lower your risk of atrial fibrillation. For example, olive oil, nuts, and dark chocolate have all been shown to decrease your risk of atrial fibrillation.
At first glance, eating more plant-based fats to prevent atrial fibrillation may seem counter-intuitive. However, there are at least two good reasons why boosting plant-based fats may be beneficial. The first is that plant-based fats, especially nuts, prevent weight gain. The second is that if your diet contains a lot of healthy fats you probably won’t get much of an atrial fibrillation promoting blood glucose spike.
4. Tripple Your Fiber (think vegetables not supplements)
Just as I tell my patients to triple their veggies, I also want them to triple their fiber intake from real food sources. Why fiber? Because fiber may also prevent atrial fibrillation.
For example, in one study researchers were able to identify a statistical trend of up to a 36% reduced risk of atrial fibrillation with fiber. Now this study was especially remarkable given that the best fiber eaters in this study (27 grams daily) couldn’t even achieve the bare minimum amounts recommended by USDA.
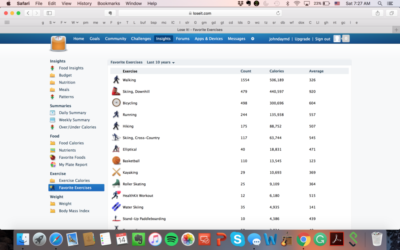
Getting more fiber from real food sources is easy to do. I have been tracking my nutrient intake for years and have observed that unless I am traveling, getting more than 100 grams of fiber daily from real food (no fiber supplements) is surprisingly easy to do.
So how can fiber help to prevent atrial fibrillation? Based on a review of 44 published studies, fiber increases your sense of feeling full by 39% which then correspondingly decreased caloric intake by 22%. Basically, the more fiber you get, the less you will weigh.
Fiber not only optimizes your body weight but it also normalizes glucose metabolism. For example, study after study has shown that blood glucose spikes can be minimized or even prevented with fiber. The key point here is that if you can triple your non-starchy veggie intake, then your fiber intake will probably triple as well.
5. Eat Fish
If you like meat, then your best choice when it comes to atrial fibrillation is the low mercury high omega 3 fatty fish otherwise known by the acronym “SMASH.” SMASH stands for salmon, mackerel, anchovies, sardines, and herring.
Like vegetables, nuts, seeds, fruit, and olive oil, fish may also be protective. For example, one study of 4,815 people showed that regular fish eaters had a 31% decreased risk of atrial fibrillation. But before you make fish part of your daily food plan, not all studies show that fish helps.
For example, in a study of 44,720 women, no benefit from fish was found. Another study showed that while fish was helpful, eating it fried wasn’t. A third study showed that eating fish in moderation was good but that eating too much of it was associated with more atrial fibrillation. And for those wishing to skip the fish and take a pill instead, fish oil isn’t helpful.
So how do you make sense of all these conflicting studies? While it may not be the best approach for everyone, here is what works for me. As fish is the healthiest meat, wild salmon is the only meat I eat. Because I don’t want to consume too much, I eat about one ounce daily (two small bites) as part of my breakfast. For the rest of the day, I only eat plant-based foods.
6. Avoid Processed and Fast Foods
This section needs little explaining. With processed and fast foods you are getting a massive dose of sugar, health-damaging fats, and salt. Inflammation, glucose, and blood pressure all shoot up within minutes of your first bite.
One thing that is not well appreciated with processed and fast foods is the salt (sodium) load. These “foods,” pack a megadose of sodium. Sodium not only raises blood pressure but through fluid retention and its myriad of effects to the kidneys may be an important cause of left atrial enlargement and scarring of the heart thus leading to atrial fibrillation. If you want to lower the sodium in your diet, you have to be willing to eat real food that doesn’t come in a box, can, jar, or fast food container.
When you consider the impact of sugar, harmful fats, and sodium it should come as no surprise that the US has the highest rates of atrial fibrillation in the world. And it is probably the lack of processed and fast foods in remote areas of Asia that account for the 10 times higher risk of atrial fibrillation that we have in the U.S. compared to that of Asia.
7. Eat Less Animal Meat and Dairy
I realize this last point will probably be highly contentious so I saved it for last. If you are are a believer in the research on TMAO production from the gut as a potential cause of atrial fibrillation, then the less animal meat and dairy you eat the better off you may be provided you are getting adequate amounts of vitamin B12, omega 3, calcium, etc. from other sources.
However, please note that elevated TMAO and atrial fibrillation have only been observed to coexist. These studies certainly don’t prove that TMAO causes atrial fibrillation. Also, we have to explain the paradox of how fish might decrease the risk of atrial fibrillation despite the fact that fish also increases TMAO production from gut bacteria.
What is an Example of the Atrial Fibrillation Diet?
Let’s face it; we live in a fast-paced modern world. It can be almost impossible for most people to grow a garden, source locally grown organic food, and take the time to prepare fresh real food. So how could you incorporate the Atrial Fibrillation Diet into your daily routine?
Breakfast
Breakfast really is the most important meal of the day but not for the reasons you usually hear. I have found with my patients that how their breakfast goes usually determines how the rest of the day will go.
Smoothies are a great way to start the day. As long as you aren’t adding any sugar, a smoothie loaded with green leafy vegetables, frozen berries, nuts, and seeds is a great way to protect your heart from atrial fibrillation.
Lunch
Salads are great for lunch and should be a daily occurrence with the Atrial Fibrillation Diet. As salad toppings can often undo any potential health-promoting effects of salads, I recommend never using commercially prepared salad dressings. Making your salad dressing is surprisingly tasty and quick. This is what we do in our home. For ideas, please look through our family’s salad dressing recipes on this website.
If you are eating out, all is not lost. Combining olive oil and balsamic vinegar makes for a great salad dressing on the go. Likewise, nuts and seeds can substitute for salad dressings as well. Personally, I try to avoid the salad dressing when eating out as you never know how much sugar, bad fats, or chemicals they have put in it.
Dinner
For dinner, we love a stir-fry vegetable dish. Sometimes some wild salmon will accompany the stir-fry. Often we will mix in some lentils, garbanzo beans, or tofu. Once again, if you are looking for ways to make lightly cooked vegetables taste delicious, here is my favorite.
If a dessert is desired, we love dark chocolate from Trader Joe’s or Whole Foods. At these two stores, there are many dark chocolate options that both taste great and come without any sugar.
The Top 4 Atrial Fibrillation Diet Guidelines
When it comes to eating, some people like rules and others don’t. Personally, I’m not one for a detailed list of “forbidden foods” or rules, rather I like general guidelines And if you have to ask, can I eat this? Then the answer is almost always no.
Eating should be an enjoyable thing that you share with friends and family. So if you can just remember these four things, then you are 90% there for following the Atrial Fibrillation Diet.
1. Triple Your Vegetable Intake
No further explanation needed here. The more veggies you eat, the healthier you will be.
2. Avoid Sugar
Once again, we’ve covered this extensively in this article. I can’t think of a single health benefit that comes from sugar.
3. Avoid Flour
Flour may come as a surprise to many readers. The reason why I have listed flour isn’t due to gluten issues but rather because flour behaves exactly like sugar in the body. Indeed, this explains why even so-called healthy whole wheat bread will spike your blood glucose faster than a Snicker’s bar! If you can’t live without bread, like me, then learn to like bread made with almond flour or without flour (Ezekiel bread or Trader Joe’s flourless bread).
4. Don’t Eat After 7 PM
Eating late causes weight gain, fouls up your glucose metabolism, and spikes your blood pressure. None of these things are good for people battling atrial fibrillation. If you can learn to stop eating by 7 PM, then you’ll also be practicing a form of intermittent fasting with additional health benefits.
Is the Ketogenic Diet Safe with Atrial Fibrillation?
Perhaps you saw the worldwide news reports that the ketogenic diet wasn’t safe for atrial fibrillation? In case you missed this media sensation, here is the most credible source to review this unpublished study.
While the headlines likely put fear in the hearts of any keto follower, the truth is that this study really doesn’t tell us much. In fact, it really wasn’t even a study of the ketogenic diet. Rather, they just looked at the atrial fibrillation risk based on a low (<45% of calories), moderate (45-52% of calories), or high carbohydrate diet (>52% of calories).
One strength of the study is that they had nearly 14,000 people with approximately 20 years of follow up. However, the data quality is highly suspect as it was based on a food questionnaire where people tried to report what they remember eating over the years. The bottom line is that the low carbohydrate group had a 16-18% increased risk of atrial fibrillation.
I suspect that the real reason why more atrial fibrillation was observed in the low carbohydrate group was that they probably had other unhealthy eating habits that increased their risk. For example, were they eating more cheeseburgers, hot dogs, or other processed foods? Perhaps there was even more alcohol or smoking in the lower carbohydrate group. Until the study is published, I can’t really comment more than this.
If the ketogenic diet is working for you, I wouldn’t stop it based on the preliminary results of this study. Rather, the more plant-based you can make your ketogenic diet the healthier it will probably be for your heart.
Final Thoughts
As Hippocrates so famously said more than 2,000 years ago, let food be your medicine. And when it comes to atrial fibrillation, I have seen first hand whether food suppresses or promotes arrhythmias. While there is no one proven best diet for atrial fibrillation, provided you aren’t overweight and you have minimized sugar, flour, and other “modern foods,” in conjunction with copious amounts of vegetables, your risk of atrial fibrillation will likely be quite low.